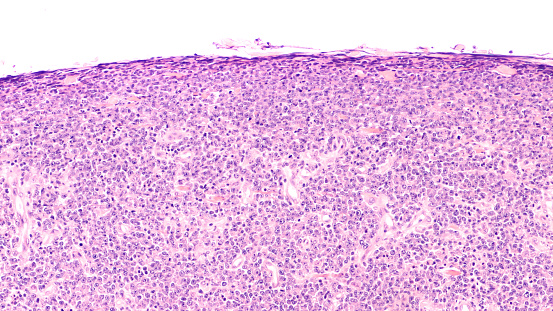
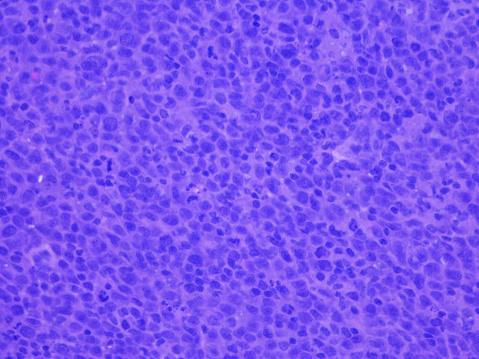
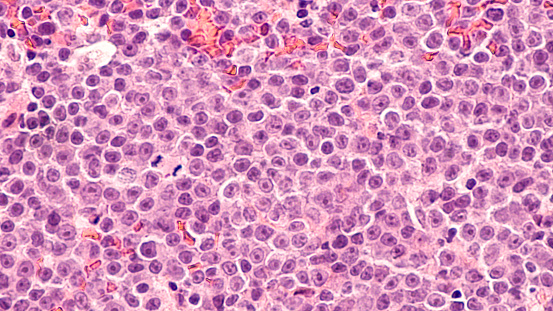
Total lesion glycolysis (TLG) and National Comprehensive Cancer Network International Prognostic Index (NCCN-IPI) can both predict survival in diffuse large B-cell lymphoma (DLBCL) of nodal origin patients, according to a study published in Quantitative Imaging in Medicine and Surgery.
The study authors assessed 184 consecutive de novo nodal DLBCL patients who underwent baseline positron emission tomography/computed tomography (PET/CT). They used Kaplan-Meier estimates to analyze the clinical, biological, and PET/CT parameters, and Cox proportional hazards modeling to evaluate the potential independent predictors for progression-free survival (PFS) and overall survival (OS).
Following 35 months of follow-up, the 3-year PFS and OS were 65.2% and 73%, respectively. A subsequent univariate analysis showed that TLG, cell-of-origin subtypes, and NCCN-IPI were both PFS and OS predictors. The results suggested that high TLG, non-germinal center B (non-GCB), and high NCCN-IPI, were all independent factors associated with worse PFS and OS.
“The TLG, cell-of-origin subtypes, and NCCN-IPI are independent prognostic survival factors in DLBCL patients. Moreover, the revised risk model composed of the number of risk factors (high TLG, non-GCB, and high NCCN-IPI) can stratify patients better than the NCCN-IPI, especially for patients at high risk, which suggests its potential integration into decision making for personalized medicine,” the researchers concluded.
Link: https://pubmed.ncbi.nlm.nih.gov/34079720/
Keywords: National Comprehensive Cancer Network International Prognostic Index, Total lesion glycolysis, cell-of-origin, diffuse large B-cell lymphoma, prognosis