Even if cancer patients are not fully ready to have an advance care planning (ACP) discussion, they may still be open to the conversation, according to a study.
ACP discussions are known to have beneficial impacts on cancer patients, but both healthcare professionals and cancer patients report that readiness to have the conversation is a significant hinderance, according to the researchers.
“A primary goal of ACP is to help ensure that patients’ medical care and treatment aligns with their personal values, goals, and preferences, especially should they become unable to articulate these preferences themselves,” they explained.
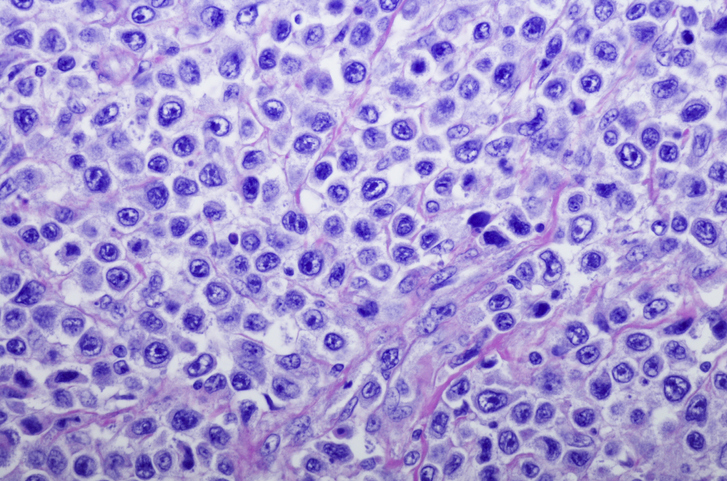
The present study was a sub-study of conversations collected for ACTION, a phase 3, international, randomized clinical trial assessing the ACTION Respecting Choices (RC) ACP intervention in Belgium, Denmark, Italy, the Netherlands, Slovenia, and the UK. The ACTION trial encompassed advanced lung and colorectal cancer patients.
The present study evaluated ACP conversations with 15 ACTION participants. The average length of the discussion was 1 hour and 25 minutes.
All 15 patients exhibited signs that they were both ready and not ready to have the ACP discussion, the study authors noted.
Signs that patients were not ready to have the ACP discussion included:
- Keeping things out of sight: Examples include “stressing the unpredictability of the future” or putting off making a decision pertaining to the future.
- Putting a stop to the discussion: The patient may simply stop engaging in the conversation.
- Limiting one’s perspective to the here and now: Rather than looking at the future, the patient only talks about the present.
- Minimizing the seriousness or significance of one’s symptoms: The patient may focus on small improvements in their health while ignoring or downplaying the more serious aspects.
- Distancing oneself from the topic being discussed: Even when the patient answers certain questions, they may divert the conversation away from themselves—making the conversation less personal or even speaking in second or third person.
On the other hand, the researchers also identified signs the patient was ready, at least to some degree, to have the ACP discussion:
- Indicating basic readiness: Not only is the patient ready to have the discussion, they are also ready to relate the conversations to themselves.
- Spontaneously mentioning ACP-related topics independently of the script prompts: The patient brings up topics of conversation without being prompted to—this suggests the patient has given this consideration outside of the discussion.
- Learning from past illness experiences: The patient can take something of value away from a past illness experience of themselves or a family member/friend.
- Demonstrating an understanding of one’s diagnosis and current state of health: The patient is able to discuss their illness on a personal level, not projecting it as if it were about someone else.
- Demonstrating and understanding of one’s disease and prognosis: The patient acknowledges the seriousness of their illness.
- Considering the topic from various sides: The patient is able to critically think about their specific scenario.
- Anticipating possible future scenarios: Looking into the future, the patient can discuss what long-term outcomes may entail, including complications and final stages of the disease.
- Accepting one’s disease and deterioration of health: The patient can openly discuss and has considered the possibility of death.
“Our study revealed that patients do not have to be ready for all elements of ACP to participate in an ACP conversation. When asked about various ACP topics, patients can respond to questions they feel ready to discuss,” the researchers concluded. They further said that certain topics in the ACP discussion may be more difficult for patients to answer than others, suggesting that “readiness should not be seen as an unequivocal prerequisite for starting an ACP conversation, but rather as a state of mind that fluctuates throughout an ACP conversation.”
The study was published in Supportive Care in Cancer.
Credit: Original article published here.