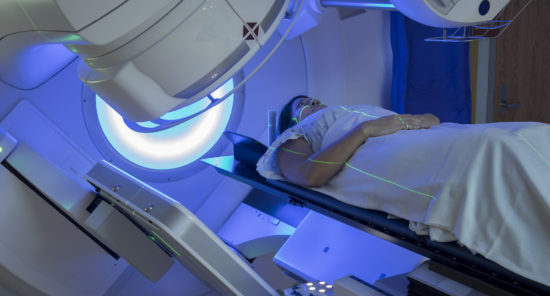
Older adults who survive breast cancer and continue long-term opioid use are at an increased risk for serious adverse drug events, a study cautioned.
“Older adults, who account for nearly two-thirds of the 16 million people who have survived cancer in the US, have high rates of opioid use for cancer pain as well as significant clinical complexities owing to their age, comorbid conditions, and cancer treatments. These characteristics may predispose this population to adverse drug events not related to opioid misuse,” the authors of the study wrote. “However, little is known about the association between active opioid therapy continuing after active cancer treatment and comprehensive opioid-related serious adverse drug events.”
They retrospectively reviewed Surveillance, Epidemiology and End Results-Medicare data spanning 2007 through 2016 on fee-for-service Medicare beneficiaries aged between 66 and 90 years diagnosed with stage 0 to 3 breast cancer from Jan. 1, 2008, through Dec. 31, 2015, who completed active treatment. Adjusted risk ratios (aRRs) were calculated for adverse drug events pertaining to substance misuse including diagnosed opioid abuse, dependence, or poisoning; adverse drug events pertaining to opioid use including gastrointestinal events, infections, falls and fractures, and cardiovascular events; and all-cause hospitalization correlated with opioid supply the day before.
Opioid Use, Especially in Higher Doses, Increases Risks for Adverse Drug Events
The study encompassed 38,310 women with a mean (SD) age of 74.3 (6.3) years. Per 1,000 person-days, there were 0.010 (95% confidence interval [CI], 0.008 to 0.011) adverse drug events related to substance misuse, 0.237 (95% CI, 0.229 to 0.245) other adverse drug events related to opioid use, and 0.675 (95% CI, 0.662 to 0.689) all-cause hospitalizations. Opioid use significantly increased the risk of adverse drug events related to substance misuse (aRR=14.62; 95% CI, 9.69 to 22.05; P<0.001) and was also associated with other adverse drug events pertaining to opioid use (aRR=2.50; 95% CI, 2.11 to 2.96; P<0.001) as well as all-cause hospitalization (aRR=2.77; 95% CI, 2.55 to 3.02; P<0.001). Women whose daily opioid doses were high, compared to those with lower daily doses, had higher risks for all of the measured outcomes. Women whose current opioid supply was ≥50 mg morphine equivalent dose per, compared to those with days with no opioid exposure, had a 3.4-fold higher risk of any adverse drug event related to substance misuse (aRR=3.40; 95% CI, 2.47 to 4.68; P<0.001); women whose daily dose was 1 to 49 mg morphine equivalent had a 2.3-fold higher risk (aRR=2.29; 95% CI, 1.89 to 2.77; P<0.001).
“Our findings add to these concerns by demonstrating that opioid therapy significantly increases the risk of multiple preventable serious adverse drug events. Clinicians should carefully weigh the benefits and comprehensive risks of opioid therapy in older adult survivors of breast cancer who have completed active breast cancer treatment,” the study authors concluded.
The study was published in JAMA Network Open.
Credit: Original article published here.