A study found that a high expression of the coding gene human leukocyte antigen-E (HLA-E) is associated with advanced disease state of multiple myeloma (MM), and HLA-E may serve as a biomarker for high-risk MM. The findings were published in Frontiers in Oncology.
Although the prognosis for MM has markedly improved as better treatment options have emerged, a certain percentage of MM patients have been profiled as high-risk for relapsed/refractory MM (RRMM), which carries reduced progression-free survival, and overall survival. Therefore, early identification of MM patients at high-risk of RRMM is paramount.
Enter HLA-E – a non-classical major histocompatibility complex (MHC) class I molecule which plays a integral role in immune response. Researchers noted that studies have shown that HLA-E expression correlates with worse progression-free survival in newly diagnosed, treatment-naïve MM patients. Thus, they wrote, “the present study aims to continue our investigation on the clinical meaning of HLA-E expression in MM patients and further explore whether peptide P3 could target HLA-E positive myeloma cells.”
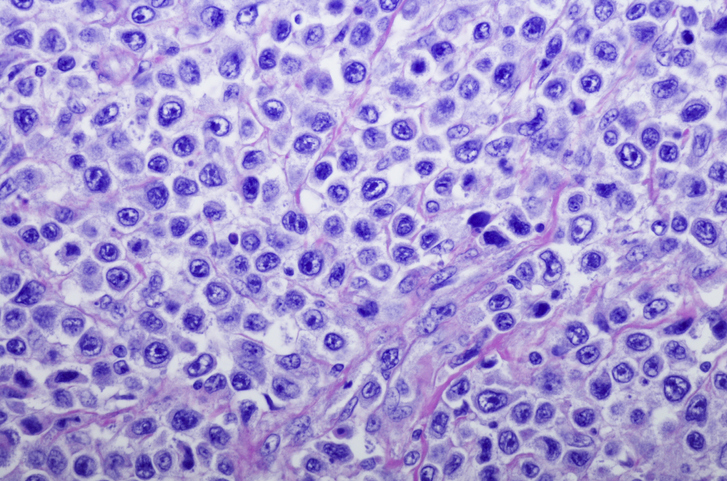
In this study, researchers assessed 30 newly diagnosed MM patients (18 males, 12 females) from January 2018 to November 2019. The researchers collated bone marrow samples following MM diagnosis, following patient consent. Exclusion criteria was stipulated as any patients who had a history of any immune deficiency disease, transplantation or other cancer, or any previous immunosuppressive therapy.
The researchers analyzed the expression of HLA-E, CD138 and CD45 using flow cytometer (FCM), which was performed on at least 50,000 cells to discern the viable ones. HLA-E expression was further assessed using CellQuest software.
According to the results, HLA-E was detected in 30 MM patients and in 7 non-malignancy control patients in FCM. In MM patients, the researchers observed that CD138 and CD38 were strongly positive in abnormal plasma cells, thus indicating that the CD138 antigen can be used to identify MM cells, the researchers noted. A quantitative analysis of FCM results showed that the mean fluorescence intensity of HLA-E was 39.27 ± 27.01 (15.4-152.61) in MM cells and 11.28 ± 0.79 (8.82-14.33) in control cells with positive CD138. The findings demonstrate that HLA-E was highly expressed in MM patients. The target-binding peptides M and P1-3, both interact with the HLA-E protein in MM cell lines, HLA-E, while P3 showed the highest affinity for impeding a key HLA-E interaction.
The researchers concluded: “The results of this study reveal the overexpression of HLA-E on MM cells, especially of high-risk patients, and the high binding frequency of peptide P3 to HLA-E on MM patients in vitro. From a therapeutic perspective, HLA-E can be considered as an effective targeting therapy against MM cells, while P3 specifically binds with HLA-E. Consequently, this interrupts the interaction between HLA-E and the inhibitory receptor NKG2A, providing a promising strategy to improve the immune clearance of MM cells.”
New research: HLA-E Binding Peptide as a Potential Therapeutic Candidate for High-Risk Multiple Myeloma: Human leukocyte antigen-E (HLA-E) has been putatively associated with the pathogenesis of multiple myeloma (MM). Our study first showed… https://t.co/Nyaqd15ZGL #oncology
— Frontiers in Oncology (@FrontOncology) June 9, 2021
Credit: Original article published here.